“Just Shave!”
(A compilation from first-person accounts)
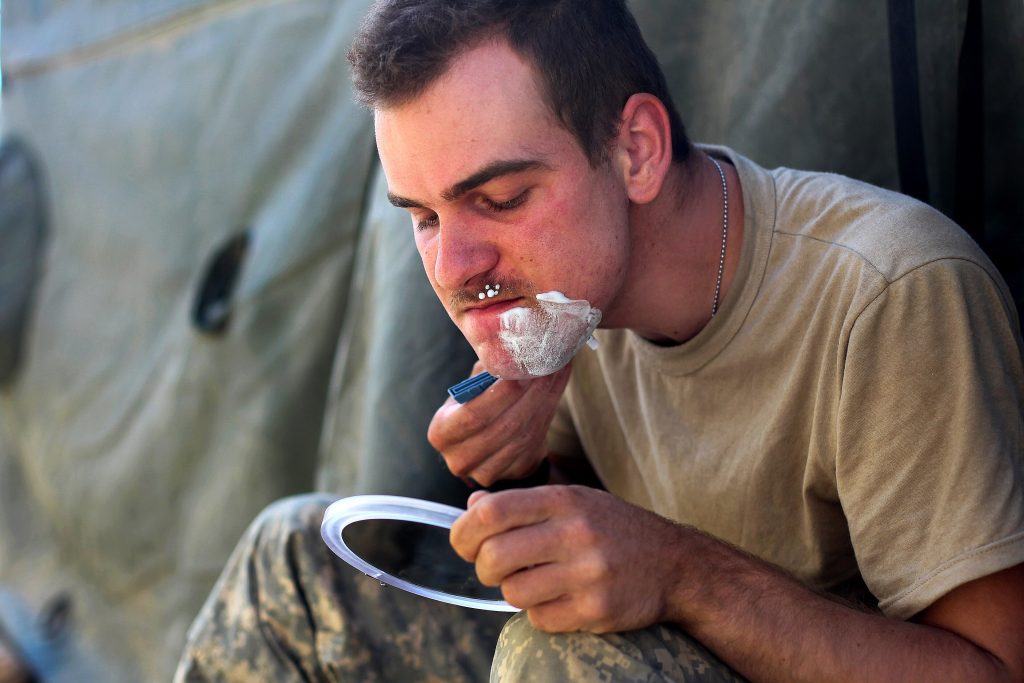
“I’ve never had the luxury of thinking shaving was no big deal.
For me, it starts burning before I even finish the shave. Not a nick, not razor burn the way most people mean it—a deep, tight heat under the skin, like it already knows what’s coming. By the end of the day, my neck feels swollen, tender, like the skin is angry.
The next morning the bumps show up.
They aren’t pimples. They’re hard, sore knots under the skin. Some have hairs trapped beneath the surface, curled back into my neck. Some don’t show anything at all—just painful lumps that hurt when I turn my head or button my collar. Shaving again doesn’t fix it. It makes it worse.
Every shave cuts the hair short and sharp. As it grows back, it curls immediately and drives itself into the skin. Now my body treats my own hair like an infection. Redness turns to swelling. Swelling turns to pus. Sometimes they open. Sometimes they bleed. Over time, scars form—dark marks that never quite go away.
And there’s no reset button.

I don’t get to let my skin heal. I don’t get to take a week off shaving. Every day restarts the same cycle: shave, burn, swell, break out, scar—then do it again.
People who don’t deal with this think it’s a hygiene issue. Or a discipline issue. Someone always says, “You just need to shave the right way.” Hot towel. Cold water. One blade. Electric razor. Special creams. Alcohol. Prescription meds.
I’ve tried all of it.
Some things help a little. None of them fix the problem as long as I’m required to shave close.
There’s also the part nobody puts in medical textbooks. People notice. Supervisors comment. Someone asks why my neck looks “messed up.” Someone jokes about razor discipline. Someone implies I’m being lazy or pushing the rules. I stop touching my face in public because it hurts—and because I don’t want the attention.
The irony is that the solution is obvious. The moment I let the hair grow even a little, my skin calms down. The burning fades. The bumps shrink. The scars stop getting worse.
But now I’m out of compliance.
So I’m stuck choosing between two bad options: follow the rule and damage my skin every day, or protect my skin and explain myself over and over again.
For me, shaving bumps aren’t a nuisance. They’re a chronic injury caused by a daily requirement—one that never heals because it’s never allowed to.”
And that’s where this conversation really starts.
Beards, Bumps, and Breathing
Facial Hair, Respirator Seals, and the Military’s Impossible Tradeoff
Every debate about military grooming standards eventually collapses into one technical claim: “It’s about the mask seal.” (Although many believe that it’s a convenient leadership fallback reason; few people want to say they are against facial hair because they just think beards look sloppy on their troops.) So let’s take a few minutes to examine the mask seal argument.
The claim is usually delivered as doctrine, not analysis. When stripped of tradition, regulation, and cultural baggage, the issue resolves into a genuine engineering and medical tradeoff involving respirator mechanics, skin health, manpower realities, and risk frequency. The problem is not whether beards look professional. The problem is that two different respiratory protection requirements exist, they operate on very different timelines, and facial hair—and the medical consequences of shaving—sit directly at their intersection.
Do respirators and gas masks seal properly with facial hair?
On average, no—and more importantly, they become less predictable. But read on.
Across decades of peer-reviewed research, tight-fitting respirators and gas masks show degraded seal performance when facial hair occupies the sealing zone—the area where the facepiece must maintain continuous contact with skin. The mechanism is simple: hair creates micro-channels that allow air to bypass the filter, especially during movement, speech, perspiration, and extended wear.
What the literature does not support is the simplistic claim that any facial hair automatically causes failure. Instead, the data shows progressive degradation and increasing variability as hair length and density increase. Variability—not absolute failure—is the real enemy of protective systems.

How well do respirators seal at various hair lengths?
The strongest length-controlled dataset comes from Floyd et al. (2018), which systematically measured respirator fit using quantitative fit testing across defined beard lengths. This study matters because it isolates hair length and density as variables rather than relying on anecdote.
The findings are unambiguous:
• ~1.6 mm stubble (0.063″)
All tests passed. Seal performance was not significantly different from clean-shaven in their penetration model.
• ~3.2 mm (0.125″)
Approximately 98% of tests passed, but overall fit factor declined and variability increased.
• ~6.35 mm (0.250″)
Pass rate dropped to roughly 81%. Failure became non-trivial even under controlled conditions.
• ~12.7 mm (0.500″)
Pass rate dropped further to approximately 58%. Failure became more likely than success.
Critically, hair density—not just length—was a statistically significant predictor of worse fit. Two individuals with the same beard length can have very different outcomes depending on hair coarseness, density, and facial geometry. This explains why some people sincerely report “passing with a beard” while others fail at similar lengths. Both can be true.
Shaving bumps (PFB): the other half of the problem
Pseudofolliculitis barbae (PFB), commonly called shaving bumps, is not a minor inconvenience. It is a medically recognized inflammatory condition caused by tightly curled hairs re-entering the skin after close shaving. The condition disproportionately affects men with curly or coiled facial hair and is highly prevalent, particularly among Black males.
Dermatology literature is consistent on one point: close shaving worsens PFB; allowing hair to grow reduces it.
Clinically recommended approaches commonly include:
• Temporarily stopping shaving until lesions resolve (often several weeks)
• Avoiding close blade shaving
• Using clippers or trimming methods that leave ~0.5–1.0 mm of hair
• In many cases, allowing growth up to ~3 mm significantly reduces recurrence
The physiological reason is straightforward: hair that is not cut flush with the skin is less likely to curl back into it. The sharp, freshly cut hair tip—not the presence of hair itself—is the primary driver of inflammation.
Where the Two Problems Collide
This is the central conflict.
Using the respirator data and dermatology guidance together, a narrow overlap emerges:
• ~1–1.6 mm hair length sits in a transitional zone where:
o Many individuals experience relief from acute PFB flares, and
o Quantitative fit testing shows high pass rates with minimal degradation
At ~1.6 mm, Floyd’s data shows a 100% pass rate under controlled conditions. That length is clinically compatible with early PFB recovery and mechanically compatible with respirator sealing—for a limited window.
But that compatibility is fragile.
Beyond ~3 mm, PFB risk continues to decline, but respirator seal reliability degrades rapidly and unpredictably. By ~6 mm, failure rates approach one in five even in controlled testing. The hair length that best protects skin health is longer than the hair length that reliably preserves a tight seal.
This is not a cultural conflict. It is a millimeter-scale biomechanical one.
Two similar problems that are not the same problem
At this point, a critical distinction must be made.
Industrial respirators: frequent, real exposure
Many service members—maintainers, fuel handlers, painters, firefighters—wear industrial respirators routinely. These exposures are:
• Frequent and predictable
• Often involve extended wear
• Accompanied by heat, sweat, motion, and repeated donning
Here, seal reliability over time matters more than theoretical peak performance. Chronic skin inflammation from daily shaving can itself undermine seal consistency and compliance. This is where the PFB-versus-seal tradeoff actually plays out day after day.
Chemical warfare gas masks: rare, catastrophic exposure
Every service member must be able to wear a gas mask for CBRN environments. But real-world chemical exposure is rare, and most personnel encounter masks primarily in training or exercises with no live agent present.
This is a low-probability, high-consequence scenario. In this context, variability is unacceptable. Worst-case assurance matters more than daily comfort or long-term skin health.
Treating these two requirements as identical obscures the real tradeoff: frequency versus consequence.
The manpower dimension
PFB is common enough that treating it as a blanket disqualifier would remove a meaningful share of the recruiting pool—particularly among Black males, where prevalence estimates in military and dermatology literature often fall between 45% and 80%, compared with low single-digit percentages among White males.
Modeling against realistic military demographic distributions, a non-waivable “no PFB” standard could plausibly exclude 10–25% of male applicants, with disproportionate impact on specific populations. That is not a grooming issue. That is a force-structure issue.

Broken skin and chemical exposure: an uncomfortable irony
Another under-acknowledged factor is skin integrity.
Chemical warfare agents—particularly vesicants—can cause injury via skin contact. While inhalation and ocular exposure are often dominant pathways, percutaneous absorption is a recognized route, and compromised skin generally allows greater penetration than intact skin.
From a biological standpoint, chronic shaving-induced skin damage is not neutral in a chemical exposure scenario. “Shave at all costs” can become self-defeating if it produces persistent inflammation, abrasions, or open lesions.
The compromise question: short hair now, shave when the threat is real?
This is where theory meets operational reality.
Two additional facts matter:
- Chemical warfare risk has historically been preceded by intelligence warning.
Modern U.S. forces have not faced credible chemical threats without indicators. CBRN posture changes have historically been driven by intelligence assessments, not instantaneous surprise exposure. - Long shifts already produce stubble.
Fourteen-hour shifts are common in many operational environments. Even under strict grooming standards, many personnel naturally reach 1–2 mm of stubble by the end of a workday. In practice, the system already tolerates short-term deviations from a perfect clean shave.
Taken together, these realities change the analysis.
Allowing up to ~3.2 mm of facial hair during routine operations—while requiring shaving upon elevation of chemical threat posture—becomes a defensible, risk-managed compromise, provided it is understood for what it is.
What this compromise does
• Reduces chronic PFB flares and skin damage
• Improves long-duration comfort and compliance during routine respirator use
• Keeps most users within a high-probability seal range for daily tasks
• Aligns with the reality that perfect shaving is not maintained across long shifts anyway
What it does not do
• It does not represent maximum CBRN readiness at all times
• It does not eliminate seal variability
• It does not protect against a zero-warning chemical event
But if zero-warning chemical exposure is not the assumed threat model, and intelligence warning is expected, then requiring shaving when the threat becomes real is operationally coherent.
In other words, this is not a loophole. It is an explicit acknowledgment that day-to-day readiness and worst-case readiness are different optimization problems.

The Honest Bottom line
• Tight-fitting respirators and gas masks do not, on average, seal as well with facial hair, and seal performance becomes increasingly unpredictable as hair length and density increase.
• Very short stubble (~1–1.6 mm) can, in many individuals, support acceptable respirator seals while reducing acute shaving-bump flare-ups—but only temporarily.
• The hair length that best protects skin health eventually undermines seal reliability.
• Industrial respirator use and chemical warfare readiness are not the same problem, and pretending they are leads to poor tradeoffs.
• Given intelligence warning timelines and real-world grooming realities, allowing limited short hair growth during routine operations—paired with shaving upon elevated chemical threat—is a reasonable, evidence-consistent compromise, not a disciplinary failure.
This is not a question of appearance.
It is a question of physics, physiology, probability, and consequence.
And none of those care what we wish the answer were.
One Final Word
The hard truth is that it is extremely difficult to advance in the U.S. military with a beard. All one has to do is look at all the senior leadership bio photos to see that even mustaches are rare. Shaving waivers have been around for decades, yet very few people advanced to senior ranks while utilizing them. So, it’s painfully obvious that it’s not just about mask seal. It’s mostly about how military leaders view what they believe to be professional appearance. How many potentially great leaders have we lost either because they weren’t advanced by commanders or they just couldn’t deal with the idea of 20 years of pain from shaving?

References
1. Floyd et al. (2018)
Floyd, E. L., Henry, J. B., & Johnson, D. L. (2018).
“Influence of facial hair length, coarseness, and areal density on seal leakage of a tight-fitting half-face respirator.”
Journal of Occupational and Environmental Hygiene, 15(4), 334–345.
2. Skretvedt & Loschiavo (1984)
Skretvedt, O. T., & Loschiavo, J. G. (1984).
“Effect of facial hair on the face seal of negative-pressure respirators.”
American Industrial Hygiene Association Journal, 45(1), 63–66.
3. Stobbe et al. (1988)
Stobbe, T. J., et al. (1988).
“Facial hair and respirator fit: A review of the literature.”
American Industrial Hygiene Association Journal, 49(4), 199–204.
4. Prince et al. (2021)
Prince, S. E., et al. (2021).
“Assessing the effect of beard hair lengths on face masks and respirators.”
Journal of Exposure Science & Environmental Epidemiology, 31(5), 769–777.
5. Taylor & Cook-Bolden (2006) (or equivalent dermatology review)
Taylor, S. C., & Cook-Bolden, F. (2006).
Pseudofolliculitis barbae: Pathogenesis and treatment.
Cutis, 78(5), 330–334.
_____________________________
Dave Chamberlin served 38 years in the USAF and Air National Guard as an aircraft crew chief, where he retired as a CMSgt. He has held a wide variety of technical, instructor, consultant, and leadership positions in his more than 40 years of civilian and military aviation experience. Dave holds an FAA Airframe and Powerplant license from the FAA, as well as a Master’s degree in Aeronautical Science. He currently runs his own consulting and training company and has written for numerous trade publications.
His true passion is exploring and writing about issues facing the military, and in particular, aircraft maintenance personnel.
As the Voice of the Veteran Community, The Havok Journal seeks to publish a variety of perspectives on a number of sensitive subjects. Unless specifically noted otherwise, nothing we publish is an official point of view of The Havok Journal or any part of the U.S. government.
Buy Me A Coffee
The Havok Journal seeks to serve as a voice of the Veteran and First Responder communities through a focus on current affairs and articles of interest to the public in general, and the veteran community in particular. We strive to offer timely, current, and informative content, with the occasional piece focused on entertainment. We are continually expanding and striving to improve the readers’ experience.
© 2026 The Havok Journal
The Havok Journal welcomes re-posting of our original content as long as it is done in compliance with our Terms of Use.



